Mushrooms represent a separate kingdom of the animal world. They come in many forms: edible, poisonous, mold, yeast, and many others. Modern science knows more than five hundred species of mushrooms. These creatures are found everywhere on our planet, even inside a person. Some of them get along well with humans and make the fungus sure to cause disease. He indulges his nature and seeks to win his place under the sun, as well as resources for further growth and development. Unfortunately, this is harmful to human health.
Definition
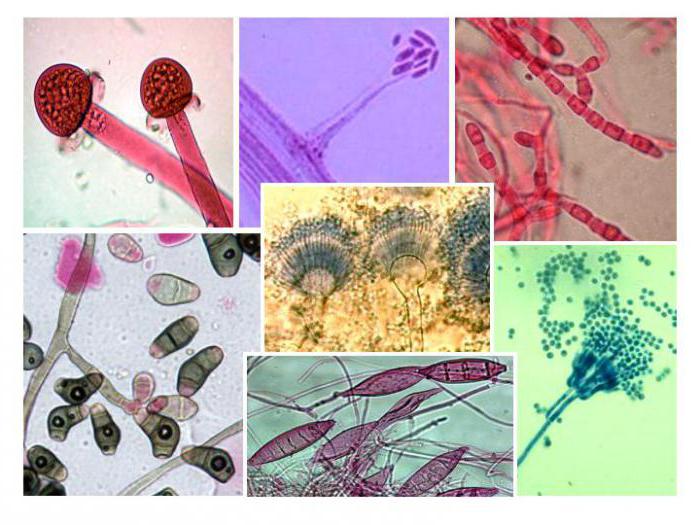
Pathogenic fungi are the causative agents of deep and superficial mycoses in humans and animals. These creatures belong mainly to the class of dermatophytes, that is, they feed on the skin. Less common among them are lower fungi and actinomycetes.
They have a certain affinity for animal tissues. This means that dermatophytes prefer the epidermis with the hairy part of the skin, yeast - the lymphatic system, candida - parenchymal organs, aspergillus live in the respiratory system, and actinomycetes love to settle in the bones.
Knowing these features, the doctor can differentiate diseases and prescribe specific treatment.
Classification of pathogenic fungi
 In the kingdom of fungi, pathogenic fungi are divided into two divisions: slime molds and true fungi. The latter is divided into seven classes, the names of which reflect their stages of development:
In the kingdom of fungi, pathogenic fungi are divided into two divisions: slime molds and true fungi. The latter is divided into seven classes, the names of which reflect their stages of development:
Cytridomycetes;
- hypocytridomycetes;
- oomycetes;
- zygomycetes;
- ascomycetes;
- basidomycetes;
- deuteromycetes.
The first four representatives form a group of lower fungi, the rest belong to the higher ones, and the last class belongs to imperfect fungi. Most pathogenic fungi that cause disease in humans are deuteromycetes.
Properties of pathogenic fungi

A person usually does not immediately notice that pathogenic fungi have entered his body. The spores (mushroom seeds) elongate and take the form of a tube that continues to grow and thinner to eventually turn into a hyphae and become the basis of the mycelium. Already at this stage, the difference is noticeable. The hyphae of the higher fungi have septa, while the lower ones do not. Hyphae from different spores grow, intertwine with each other and eventually mycelium grows on the substrate.
For the diagnosis and production of drugs, pathogenic fungal species are grown on such as Sabouraud, Czapeka-Doksa, on wort and wort agar. A prerequisite is a pH below seven.
Mushroom cells are covered with a wall of carbohydrates, but chitin remains the substance by which species can be determined. It does not interact with penicillins and lysozyme, therefore it has greater virulence for the human body.
The pathogenic fungus is resistant to physical and chemical disinfectants. Treatment from them can cause irreparable harm to human organs and systems, since a high concentration of drugs in body fluids is required. The most sensitive to therapy are microspores, and the least - candida. The selection of drugs is complicated by the fact that different combinations of antigens are possible in one type of fungus, and toxins, enzymes, and other pathogenicity factors are still unknown.
Features of infection in humans
Fungi that are pathogenic to humans can cause diseases that can be divided into four groups according to localization:
- Deep mycoses are damage to parenchymal organs, sepsis, dissemination of spores from the focus of the disease to neighboring tissues.
- Subcutaneous mycoses, they are subcutaneous. Mushrooms inhabit the epidermis, dermis, subcutaneous fat, fascia and even bones.
- Epidermomycosis or dermatomycosis occurs on derivatives of the upper layer of the skin: hair and nails.
- Superficial mycoses (keratomycosis). Pathogenic fungi on the skin affect only the stratum corneum and hair.
A separate group is distinguished diseases, the causative agents of which are opportunistic fungi. These are opportunistic diseases that appear when the body's immune defenses are weakened, such as HIV, hepatitis B or C, cancer.
Most often, the causative agents of mycosis are found in the soil or dust, so it is important to work in respirators, wash vegetables and herbs, and carry out wet cleaning in the premises. Deep mycoses appear after inhalation of the pathogen, and for the development of skin diseases it is necessary that the spores fall on the wound surface.
Immunity
A pathogenic fungus, entering the body, causes a cascade of immune system reactions necessary to identify the antigen and develop specific protection against it.
As a rule, all mushrooms are strong immunogens, so people often have an allergy to them. The reaction develops according to or cytotoxic type. In addition, T-helpers stimulate tissue macrophages to eliminate spores. Humoral reactions are manifested in the form of a high titer of antibodies, which can be used to determine the stage of development of the infection, as well as in the form of activation of the complement system along the classical and alternative pathways.
Diagnosis of mycoses

The easiest way to identify a pathogenic fungus is microscopy. Blood, mucus, and skin are taken from patients from affected areas, applied to glass slides, stained or treated with acids, and then placed under a light or electron microscope. This procedure allows you to consider the morphological features of the pathogen and determine its type.
Sometimes in the laboratory, fungi are sown on selective media and observed for their growth and fermentation of various substances. This helps to identify the pathogen from a biochemical point of view.
In response to the introduction of pathogenic fungi, antibodies appear in human blood, the presence of which can be determined by serological research methods. However, the result of such a procedure may be inaccurate, since different types of fungi contain cross-reactive antigens.
In epidemiological studies, in order to identify the part of the population that has already been ill, skin tests were used. This made it possible to find out whether the organism had previously encountered this type of antigen or not. This method cannot be used for diagnostics, as it has a low specificity.
Candida genus
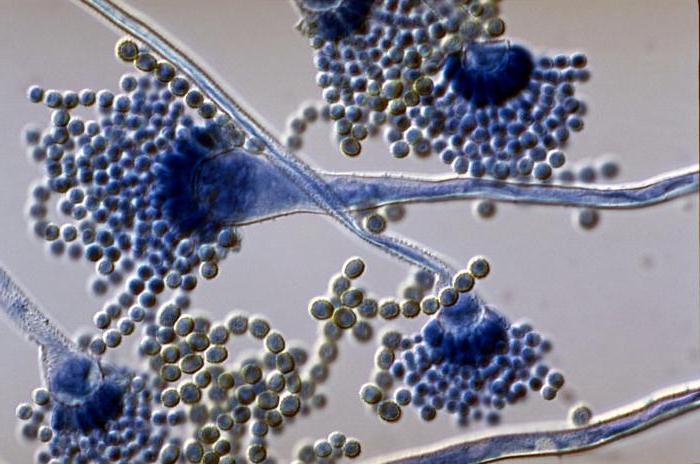
To date, 186 species of the genus Candida have been isolated, but only a few of them can cause disease in humans. For example, C. albicans, C. pseudotropicalis, C. tropicalis, C. krusei, C. parapsilosis, C. Quillermondii and others.
These are conditionally pathogenic fungi that are constantly found in the human intestine. They grow well on media rich in carbohydrates. Colonies consist of small oval cells intertwined with mycelial filaments. They multiply very quickly in the blood at a normal temperature of 37 degrees, in three hours thousands of new hyphae are formed from several spores. The germination of cells in the tissue is accompanied by a strong local immune reaction with the formation of pus.
In a healthy person and animals in the oral cavity, in 50 percent of cases they are sown in feces - almost always, on the skin and mucous membranes of the genital tract - up to 10 percent. Whether the disease develops depends largely on the state of the immune and endocrine systems. Candidiasis can be provoked by drug therapy with immunosuppressants, glucocorticosteroids, cytostatics, radiation sickness, long-term antibiotic treatment, cancer, and oral contraceptives.
Pathogenic fungi cause diseases against the background of diabetes mellitus, dysfunction of the endocrine glands and others. Recently, the number of iatrogenic candidiasis after surgical and diagnostic interventions has increased significantly. In addition, damage to the skin and mucous membranes by a fungus of the genus Candida is one of the markers of AIDS.
Pneumocystis pneumonia

Pneumocystis carinii is a fungus that primarily infects the tissues of the respiratory system. In order to look at its cultural properties, conventional culture media are not enough, it is necessary to use chicken embryos or transplanted cell cultures.
Cysts are round cells with basophilic bodies visible inside. Young and intermediate forms are always located in the colony around mature cysts. The presence of intracellular bodies allows scientists to attribute pneumocysts to the class of actinomycetes.
These fungi cause pneumonia, but in some cases other internal organs may also be affected: the kidneys, spleen, lymphatic system, retina, heart, liver, pancreas, and even the brain. Infection, as a rule, occurs in children against the background of reduced immunity.
Aspergillosis
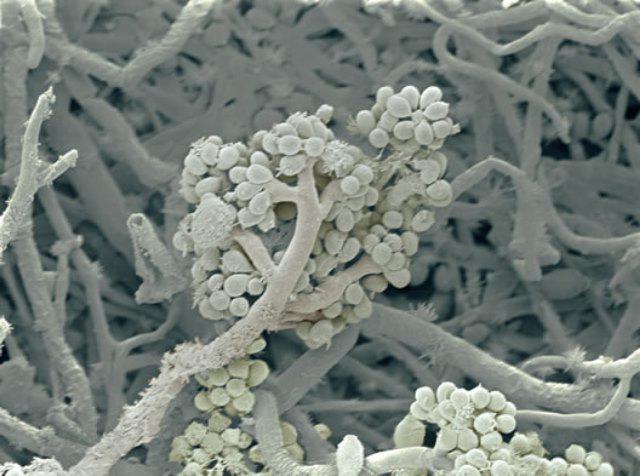
This fungus forms smooth, green colonies that grow well at human body temperature but do not tolerate heat well. Often found in food products, wood. They cause an acute infection after a large number of spores enter the human body along with food, such as bread. Often the disease develops a second time, against the background of blood pathologies, sarcoma, tuberculosis, therapy with corticosteroids, immunosuppressants. It is not transmitted from person to person.
Most often affects the respiratory system, sometimes causes skin diseases such as eczema. Around the mycelium, the tissues become necrotic, and granulomas appear in the lesion. A characteristic feature is the appearance of cavities in the affected areas, which contain fungal balls. The literature describes cases of generalized infection with damage to the central nervous system.
