2. Diseases caused by bacteria
Typhoid fever
Typhoid fever is an acute infectious disease from the group of anthroponoses. The causative agent is typhoid bacillus. Incubation period– 10–14 days. The coincidence of the clinical cycles of typhoid fever with certain cycles of anatomical changes in lymph formations intestine served as the basis for constructing a scheme morphological changes by stages.
At the first stage of morphological changes, which usually coincides with the 1st week of the disease, in lymphatic apparatus intestines, there is a picture of the so-called cerebral swelling - inflammatory infiltration of Peyer's patches and solitary follicles.
In the second stage, corresponding to the 2nd week of the disease, necrosis of the swollen Peyer's patches and solitary follicles occurs (the necrosis stage). Necrosis usually captures only the surface layers of the lymphatic apparatus of the intestine, but sometimes it can reach the muscular and even the serous membrane.
In the third stage (the period of ulceration), approximately corresponding to the 3rd week of the disease, the dead areas of Peyer's patches and solitary follicles are rejected and ulcers form. This period is dangerous with possible severe complications ( intestinal bleeding, perforation).
The fourth stage (the period of pure ulcers) corresponds to the end of the 3rd and 4th weeks of the disease; in this period, the bottom of the typhoid ulcer becomes wide, it is cleared and covered with a thin layer of granulation tissue.
The next phase (the period of ulcer healing) is characterized by the process of ulcer healing and corresponds to the 5-6th week of the disease.
Morphological changes may extend to the large intestine, gallbladder, liver. At the same time, ulcers characteristic of typhoid fever are found on the mucous membrane of the gallbladder, and typhoid granulomas are found in the liver; the disease proceeds with symptoms of damage to these organs (jaundice, acholic stools, increased content bilirubin in the blood, etc.). Intestinal injury in typhoid fever and paratyphoid is always combined with the defeat of regional lymph glands mesentery, and often - and retroperitoneal glands. Under microscopy, the same macrophage reaction is noted in them, as in the lymphatic apparatus of the intestinal wall. In the enlarged lymph nodes of the mesentery, foci of necrosis are observed, in some cases, capturing not only the main mass of the lymph node, but also passing to the anterior sheet of the abdominal integument, which can cause a picture of mesenteric-perforative peritonitis. Others may be affected The lymph nodes- bronchial, paratracheal, mediastinal. The spleen in typhoid fever is enlarged as a result of blood filling and inflammatory proliferation of reticular cells with the formation of specific granules. The liver is swollen, soft, dull, yellowish on the cut, which is associated with the severity of parenchymal degeneration. A cloudy swelling is found in the kidneys, sometimes necrotizing nephrosis, less often hemorrhagic or embolic nephritis; not uncommon inflammatory processes V urinary tract. IN bone marrow there are areas of hemorrhage, typhoid granulomas, and sometimes necrotic foci. Are celebrated degenerative changes in the heart muscle. Pathological changes in the lungs in typhoid-paratyphoid diseases are in most cases inflammatory. Hyperemia is found meninges and cerebral edema.
salmonellosis
Salmonellosis is an intestinal infection caused by salmonella; refers to anthropozoonoses.
With the most common gastrointestinal form of salmonellosis, the presence of edema, hyperemia, small hemorrhages and ulcerations in the mucosa of the gastrointestinal tract is macroscopically detected. Histologically detected: excessive secretion of mucus and desquamation of the epithelium, superficial necrosis of the mucous membrane, vascular disorders, nonspecific cell infiltration, etc. Except these changes, with severe and septic forms diseases, signs of dystrophy and foci of necrosis in the liver, kidneys and other organs are often observed. The reverse development of morphological changes in most patients occurs by the 3rd week of illness.
Dysentery
Dysentery is an acute intestinal infectious disease with a predominant lesion of the large intestine and intoxication. Macroscopically, the intestinal lumen contains semi-liquid or mushy masses mixed with mucus and sometimes streaked with blood. The intestine is slightly elongated in places, spasmodic in other areas. The mucous membrane is swollen, unevenly full-blooded, covered with large flakes of mucus or more evenly distributed and less viscous contents. After its elimination, small hemorrhages and shallow ulcerations at the tops of the folds are distinguishable. Lymph nodes of the mesentery grow in size, become reddish. All changes are focal character.
Cholera
Cholera is an acute infectious disease (anthroponosis) with a primary lesion of the stomach and small intestine. The causative agents are Koch's Asian cholera vibrio and El Tor vibrio. The pathological anatomy of cholera consists of local and general changes.
Local transformations are formed (mainly) in small intestine. The first 3-4 days are designated as the algid (cold) stage of cholera. The mucous membrane of the small intestine is full-blooded, edematous, with small hemorrhages throughout. Microscopically visible desquamation of the epithelium of the villi. Many vibrios are found in the intestinal wall. In general, the changes correspond to the picture of the most acute serous or serous-desquamative enteritis. The lymph nodes of the mesentery are somewhat enlarged. The peritoneum is plethoric, dry, with petechial hemorrhages. Occurrence on it and between the loops is characteristic small intestine sticky plaque, stretching in the form of threads, consisting of strands of desquamated mesothelium. Dense dark red blood in blood vessels, cavities of the heart, on sections of parenchymal organs. Serous membranes dry, covered with sticky mucus, stretching in the form of threads. Dry full-blooded peritoneum with pinpoint hemorrhages and its inherent sticky coating between the loops of the small intestine, consisting of strands of desquamated mesothelium. The spleen is reduced, the follicles are atrophic, the capsule is wrinkled. In the liver, dystrophic processes develop in hepatocytes, foci of necrosis are formed in the parenchyma. Bile formation is disturbed. The gallbladder is enlarged in size, filled with transparent light bile - "white bile". The kidney acquires characteristic appearance(the so-called motley kidney) - the cortical layer swells, pale, and the pyramids fill with blood and acquire a cyanotic hue. As a result of anemia of the cortex, severe dystrophy develops in the epithelium of the convoluted tubules, leading to necrosis, which can contribute to oliguria, anuria and uremia. The loops of the small intestine are stretched, in its lumen there is a large amount (3–4 l) of a colorless liquid that is odorless, reminiscent of “rice water”, without admixture of bile and the smell of feces, sometimes similar to “meat slops”. The liquid contains in large numbers cholera vibrios.
Microscopically, during the algidic period in the small intestine, there is a sharp plethora, swelling of the mucous membrane, necrosis and desquamation of epithelial cells - villi, resembling "faded dandelion heads" (N. I. Pirogov). In the mucous and submucosal layer - cholera vibrios in the form of "flocks of fish". There is hyperplasia of solitary follicles and Peyer's patches. In the striated muscles, foci of waxy necrosis sometimes occur. in the head and spinal cord, in the cells of the sympathetic nodes, dystrophic, sometimes inflammatory phenomena occur; there may be hemorrhages in the brain tissue. Nisslev granularity, swollen and partially subjected to degranulation, is noted in many cells; hyalinosis is noted small vessels, especially venules.
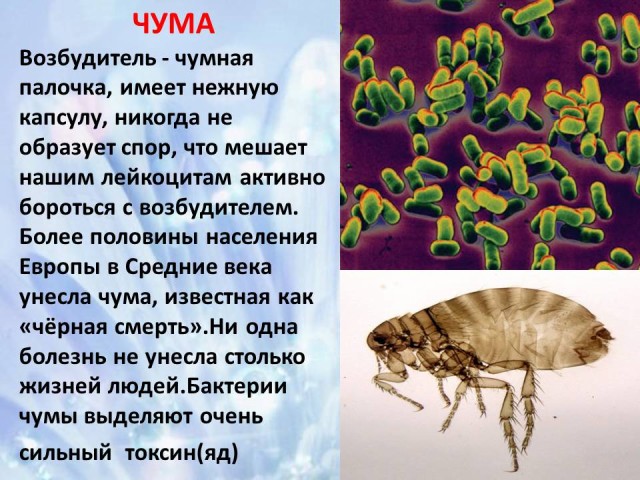
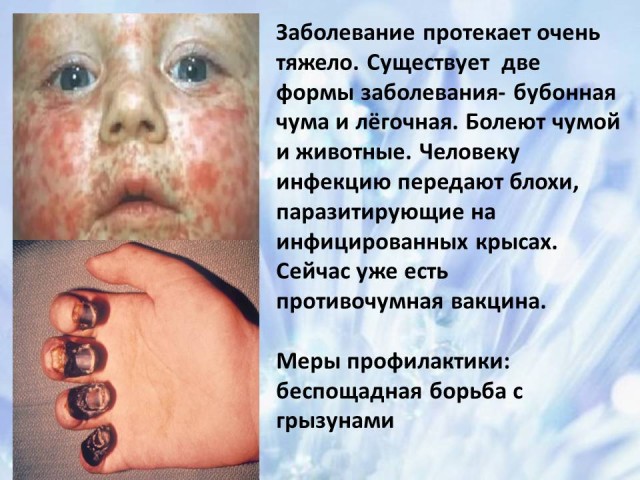
Plague
Plague is an acute infectious disease caused by the plague bacillus. There are bubonic, skin-bubonic (skin), primary pulmonary and primary septic forms of plague:
1) Bubonic plague characterized by an increase in regional lymph nodes, usually inguinal, less often - axillary and cervical. Such lymph nodes are called primary plague buboes of the 1st order. They are enlarged, soldered, testate, immobile, dark red in color with foci of necrosis. Edema develops around the bubo. Microscopically, a picture of acute serous-hemorrhagic lymphadenitis is observed, a mass of microbes accumulates in the tissue. Proliferation of reticular cells is characteristic. With the formation of foci of necrosis, lymphadenitis acquires a hemorrhagic-necrotic character. Due to the development of necrosis, purulent inflammation and melting of the tissue of the lymph node, ulcers are formed, which, with a favorable result, are scarred. With the lymphogenous spread of the infection, new buboes appear (primary buboes of the 2nd, 3rd order, etc.), where the same morphological changes are observed as in the regional lymph node. Hematogenous development of infection leads to the rapid development of plague bacteremia and septicemia, which are manifested by rash, multiple hemorrhages, hematogenous lesions of the lymph nodes, spleen, secondary plague pneumonia, dystrophy and necrosis of parenchymal organs. The rash may take the form of pustules, papules, erythema, with the obligatory formation of hemorrhages, necrosis and ulcers. Multiple hemorrhages are observed in the serous and mucous membranes. With hematogenous lesions of the lymph nodes, secondary buboes appear (serous-hemorrhagic, hemorrhagic-necrotic lymphadenitis). The spleen is enlarged 2-4 times, septic, flabby, foci of necrosis are formed, a leukocyte reaction to necrosis is observed. secondary pneumonia, arising as a result of hematogenous infection, has a focal character. A large number of dark red foci with areas of necrosis is a serous-hemorrhagic inflammation, where many pathogens are found. In parenchymal organs, dystrophic and necrotic changes can be observed;
2) the skin-bubonic (skin) form of the plague differs from the bubonic one in that the primary affect occurs at the site of infection. It is represented by a "plague conflict" (a vial with serous-hemorrhagic contents), or a plague hemorrhagic carbuncle. Lymphangitis is found between the primary affect and the bubo. At the site of the carbuncle, edema, thickening of the skin, which becomes dark red, are noted;
3) primary pneumonic plague is extremely contagious. With primary pneumonic plague, lobar pleuropneumonia occurs. Pleurisy serous-hemorrhagic. At the very beginning of the disease, with the existing plethora of lung tissue, foci of serous-hemorrhagic inflammation are formed. During the development of the disease, stasis, hemorrhages, foci of necrosis and secondary suppuration are formed. Multiple hemorrhages in the internal organs;
4) primary septic plague is characterized by a picture of sepsis without visible entry gates of infection with a very severe course. Significantly pronounced hemorrhagic syndrome(hemorrhages in the skin, mucous membranes, internal organs).
anthrax
Anthrax is an acute infectious disease characterized by a severe course in which skin lesions and internal organs; belongs to the group of anthropozoonoses. The causative agent of anthrax is the immobile bacterium Bacterium anthracis, which forms highly resistant spores: they remain in water and soil for decades. There are the following clinical and anatomical forms of anthrax:
1) skin (conjunctival, as a kind of skin);
2) intestinal;
3) primary pulmonary;
4) primary septic.
The cutaneous form is very common. Morphologically, it manifests itself as an anthrax carbuncle. It is based on serous-hemorrhagic inflammation. Practically together with a carbuncle, regional serous-hemorrhagic lymphadenitis occurs. Lymph nodes are significantly enlarged, dark red on section. There is a sharp plethora, edema and hemorrhage in the tissue in which it is found large cluster microbes. Loose tissue near the lymph nodes is edematous, with areas of hemorrhage. Most often the outcome skin form- recovery, but in 25% of cases sepsis develops. The conjunctival form, as one of the types of skin, develops when spores enter the conjunctiva and is characterized by serous-hemorrhagic ophthalmitis, swelling of the tissue around the eyes. In the intestinal form of the disease in lower section ileum extensive areas of hemorrhagic infiltration and ulcers are formed, serous-hemorrhagic ileitis is formed. In the lymph nodes of the mesentery, regional serous-hemorrhagic lymphadenitis occurs. intestinal form most often complicated by sepsis. The primary pulmonary form is characterized by hemorrhagic tracheitis, bronchitis and serous-hemorrhagic focal or confluent pneumonia. The lymph nodes of the roots of the lungs swell, increase, foci of hemorrhages are observed, which is associated with serous-hemorrhagic inflammation. The primary pulmonary form is often complicated by sepsis. The primary septic form is characterized by general manifestations of infection in the absence of local disorders. General manifestations are the same both in primary sepsis and in secondary, complicating skin, intestinal or primary pulmonary forms of the disease. The spleen is enlarged and flabby, dark cherry in color, almost black on the cut, gives abundant scraping of the pulp. Hemorrhagic meningoencephalitis develops. soft shells the brain are edematous, saturated with blood, have a dark red color (“red cap” or “cardinal's cap”). Microscopically, there is a serous-hemorrhagic inflammation of the membranes and tissue of the brain with a characteristic destruction of the walls of small vessels, their rupture, and the accumulation of a huge number of microbes in the lumen of the vessels.
Tuberculosis
Tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis. Pathologically, there are 3 main types:
1) primary tuberculosis;
2) hematogenous tuberculosis;
3) secondary tuberculosis.
The classical form of the morphological manifestation of primary tuberculosis is the primary tuberculosis complex. In 90% of cases, the foci of the formation of the primary tuberculosis complex are the upper and middle sections of the lungs, but it is also possible in the small intestine, bones, etc. In the primary pulmonary affect, alveolitis develops, which is quickly replaced by the typical development of cheesy necrosis. In the center of the primary affect, caseosis is formed, along the periphery - elements of nonspecific inflammation. The primary pulmonary focus is most often located directly under the pleura, so the pleura is often involved in a specific process. In the lymphatic vessels, expansion-infiltration of the walls and the appearance of tubercles occur. Elements of inflammation appear in the regional lymph nodes, turning into specific caseous changes with necrosis. Perifocal inflammation around the lymph nodes extends to the tissue of the mediastinum and adjacent lung tissue. In terms of the severity of the lesion, the process in the lymph nodes exceeds the changes in the area of primary affect, so reparative changes in the lymph nodes proceed more slowly.
There are 4 phases of the course of primary pulmonary tuberculosis:
1) pneumonic;
2) resorption phase;
3) sealing phase;
4) formation of the center of Gon.
In the first phase (pneumonic), a focus of broncholobular pneumonia (pulmonary affect) is determined, ranging in size from 1.5–2 to 5 cm. The shape of the pulmonary affect is round or irregular, its character is heterogeneous, the contours are blurred. At the same time, enlarged hilar lymph nodes are determined, an increase in the broncho-vascular pattern between the focus and lung root- lymphangitis.
In the second phase of resorption (bipolarity), a decrease in the zone of perifocal inflammation is observed, a centrally located caseous focus is more clearly revealed. Inflammatory changes in the regional lymph nodes in the region of the bronchopulmonary vessels are reduced.
In the third phase (seals), the primary focus is well defined, its contours are clear, along the periphery of the focus, calcification in the form of small crumbs begins; marginal calcification is also present in the bronchopulmonary lymph nodes.
In the fourth phase (formation of the focus of Gon), at the site of the focus of broncholobular pneumonia, calcification becomes compact, the focus acquires a rounded shape and even clear contours, its size does not exceed 3-5 mm. Such a formation is called the focus of Gon.
Outcomes of the primary tuberculosis complex:
1) healing with encapsulation, calcification or ossification;
2) progression with development various forms generalization, accession nonspecific complications atelectasis, pneumosclerosis, etc.
Hematogenous generalization develops when Mycobacterium tuberculosis enters the blood. A prerequisite for hematogenous generalization is a state of hyperergy. Depending on the state of the primary tuberculosis complex, early generalization is distinguished, which manifests itself in the form of:
1) generalized miliary tuberculosis with a massive rash of productive or exudative nodules in all organs;
2) focal tuberculosis with the formation in different bodies up to 1 cm in diameter of caseous foci.
Foci of hematogenous generalization can be a source of development of tuberculosis in various organs.
With the progression of hematogenous disseminated tuberculosis, caverns are formed. Caverns are formed as a result of cheesy decay and melting of necrotic masses. In the hematogenous form of pulmonary tuberculosis, the cavities are thin-walled, multiple and are located symmetrically in both lungs. Damage plays a role in the origin of such cavities. blood vessels, their thrombosis and obliteration. The nutrition of the affected areas of the lungs is disturbed and destruction is formed according to the type trophic ulcers. With the formation of caverns, the possibility of bronchogenic seeding of healthy areas of the lungs opens up.
There are 7 forms of secondary tuberculosis: acute focal, fibrinose-focal, infiltrative, acute cavernous, cirrhotic tuberculosis, caseous pneumonia and tuberculoma.
Sepsis
Sepsis is a common infectious disease that occurs due to the existence of a focus of infection in the body. Main morphological features sepsis are severe dystrophic and necrobiotic changes in the internal organs, inflammatory processes varying degrees expression in them, as well as a significant restructuring of organs immune system. Sepsis has the most typical morphological picture with septicopyemia. As a rule, in all observations, a primary septic focus is clearly recorded, localized at the entrance gate. In the tissues of this focus is great amount microbial bodies, intensive infiltration by leukocytes and areas of necrosis are recorded, signs of acute phlebitis or thrombophlebitis are determined. A characteristic sign of septicopyemia is the presence in many organs of metastatic purulent foci, which can often be detected with the naked eye. However, often these foci are found only under a microscope in the form of small foci, usually near blood or lymphatic vessels with vasculitis. Another typical sign of septicopyemia is dystrophic and necrotic changes in the internal organs, the severity of which often depends on the duration of the disease.
At the onset of the disease, hyperplastic manifestations predominate, which is accompanied by an increase in their size and an increase in the area of functional areas, and with a longer course of the disease, immunogenesis organs show destructive processes, accompanied mass death immunocompetent cells with practically complete exhaustion all organs of the immune system. The most typical are changes in the spleen ("septic spleen"). It is enlarged, flabby, cherry-red in section. Another variant of sepsis - septicemia - is characterized by significant features. As a rule, a fulminant course is typical for this form of sepsis.
Main morphological trait septicemia - generalized vascular disorders: stasis, leukostasis, microthrombosis, hemorrhage. The primary septic focus at the entrance gate does not always have a clear picture and is often not detected (cryptogenic sepsis). Metastatic foci typical of septicopyemia are not detected, although in some cases small inflammatory infiltrates are recorded in the stroma of some organs. Characterized by severe destructive processes in parenchymal organs and hyperplastic changes in the organs of immunogenesis (in particular, "septic spleen"). However, the effectiveness of the functioning of the immune system is low and microscopic examination a picture of incomplete phagocytosis is revealed.
Septicemia is often considered in connection with bacterial (septic) shock, which is caused mainly by gram-negative flora and proceeds with gross microcirculation disorders, blood shunting. Deep ischemia of the internal organs, caused by vascular disorders, leads to necrotic processes in many organs (in particular, cortical necrosis of the kidneys, etc.).
Pulmonary edema, hemorrhages and erosions in the gastrointestinal tract are typical. Patients with sepsis die from septic shock.
Syphilis
Syphilis, or lues, is a chronic infectious sexually transmitted disease caused by Treponema pallidum. Pale treponemas get on the skin or mucous membranes healthy person; through the existing microcracks in the stratum corneum, and sometimes through the intercellular gaps of the intact integumentary epithelium, there is a rapid penetration into the tissues.
Pale treponemas multiply intensively at the site of introduction, where, approximately a month after the incubation period, primary syphiloma (hard chancre) is formed - the first clinical manifestation syphilis. At the same time, infectious agents enter the lymphatic clefts, where they multiply rapidly and lymphatic vessels are starting to spread. Some infectious agents penetrate into the bloodstream and into the internal organs. Reproduction of pale treponemas and their promotion along the lymphatic pathways also occurs after the formation of primary syphiloma in the primary period of syphilis. At this time, there is a consistent increase in lymph nodes (regional adenitis), close to the entrance gate, and then more distant (polyadenitis). At the end of the primary period, pale treponemas multiplied in the lymphatic tract through thoracic duct penetrate into the left subclavian vein and are carried by blood flow in large quantities to organs and tissues.
The secondary period of syphilis occurs after 6-10 weeks and is characterized by the appearance of syphiloids - multiple inflammatory foci on the skin and mucous membranes. Depending on the intensity of inflammation and the predominance of exudative or necrobiotic processes, 3 types of syphiloids are distinguished: roseola, papules and pustules. They are rich in treponemes. After their healing, small scars remain.
Tertiary syphilis develops after 3–6 years and is characterized by chronic diffuse interstitial inflammation that occurs in the lungs, liver, aortic wall, and testicular tissue. Along the course of the vessels, a cellular infiltrate is observed, consisting of lymphoid and plasma cells.
Gumma is a focus of syphilitic productive-necrotic inflammation, syphilitic granuloma; can be single or multiple.
| |
Human diseases caused by bacteria
In the human body pathogenic bacteria feed, multiply rapidly and poison the body with the products of their vital activity.
Bacteria cause typhus, cholera, diphtheria, tetanus, tuberculosis, tonsillitis, meningitis, glanders, anthrax, brucellosis and other diseases.
One of these diseases a person can become infected when communicating with the patient through the smallest droplets of saliva when talking, coughing and sneezing, others - when eating food or water, which got pathogenic bacteria.
Unsanitary conditions, dirt, large crowding of people, non-compliance with the rules of personal hygiene create favorable conditions for the rapid reproduction and spread of pathogenic bacteria. This can cause an epidemic, i.e. mass disease of people.
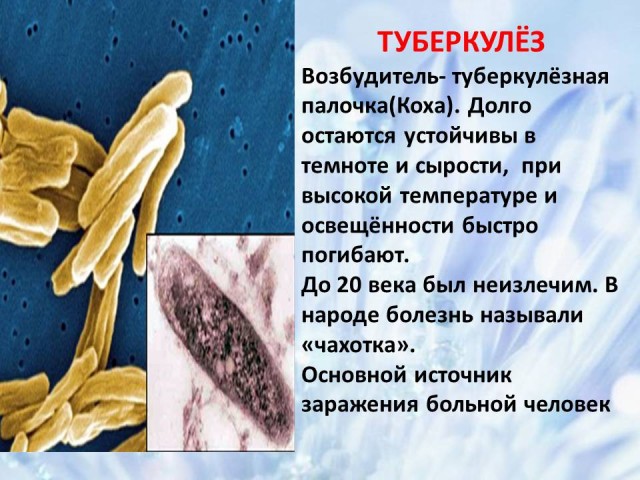
When infected tuberculosis bacillus a person gets sick tuberculosis: in the lungs, kidneys, bones and some other organs, small tubercles develop, prone to decay. Tuberculosis is a disease that can last for years.
Tuberculosis bacillus in the lungs
Plague- one of the most serious illnesses- summon plague sticks. Plague is the most fleeting disease. Sometimes only a few hours pass from the first felt signs of illness to death.
The devastating plague epidemics in antiquity were the most terrible disaster. There were cases when entire cities and villages died out from the plague.
Associated with pathogenic streptococci and staphylococci purulent diseases - for example, furunculosis, streptococcal tonsillitis.
Pathogenic bacteria also cause diseases in animals and plants.
In animals, bacteria cause diseases such as glanders, anthrax, and brucellosis. Humans can also become infected with these diseases, so, for example, in areas where livestock is sick with brucellosis, raw milk should not be eaten.
About 300 species of bacteria are known to cause various diseases plants. They cause great damage to crop and field crops, causing wilting, rotting of stems, leaf spot, etc.

Measures to combat pathogenic bacteria
There are special measures to prevent contagious diseases caused by pathogenic bacteria. Strict medical supervision for water sources and food products. At waterworks, water is purified in special sedimentation tanks, passing it through filters, chlorinated, ozonated.
Patients receive drugs that kill disease-causing bacteria. To destroy bacteria in the room where the infectious patient is located, disinfection is carried out, i.e. spraying or fumigation chemicals causing bacteria to die.
Typhoid fever
Typhoid fever is an acute infectious disease
from the group of anthroponoses. The causative agent is typhoid
wand. The incubation period is 10-14 days. Coincidence
clinical cycles of typhoid fever with
certain cycles of anatomical changes in
lymphatic formations of the intestine served
the basis for constructing a scheme of morphological changes according to
stages.
At the first stage of morphological changes, according to
term coinciding usually with the 1st week of the disease, in
in the lymphatic apparatus of the intestines, a picture is observed so
called cerebral swelling - an inflammatory
infiltration of Peyer's patches and solitary follicles.
In the second stage corresponding to the 2nd week
diseases, necrotization of swollen Peyer's
plaques and solitary follicles (stage of necrosis). Necrosis
usually captures only the surface layers
the lymphatic apparatus of the intestine, but sometimes it can
reach the muscular and even the serous membrane.
In the third stage (the period of formation of ulcers), approximately
corresponding to the 3rd week of the disease, occurs
rejection of dead areas of Peyer's patches and
solitary follicles and ulceration. This period
dangerous with possible severe complications (intestinal
bleeding, perforation).
Fourth stage (period of clean ulcers)
corresponds to the end of the 3rd and 4th weeks of the disease; V
this period, the bottom of the typhoid ulcer becomes
wide, it is cleaned and covered with a thin layer
granulation tissue.
The next phase (the period of healing of ulcers)
characterized by the healing process of ulcers and
corresponds to the 5-6th week of illness.
Morphological changes may spread
on the large intestine, gallbladder, liver. At the same time, on
mucosa of the gallbladder is found
ulcers characteristic of typhoid fever, and in the liver -
typhoid granulomas; the disease progresses with
symptoms of damage to these organs (jaundice, acholic
stool, elevated blood levels of bilirubin, etc.).
Bowel injury in typhoid fever and paratyphoid fever
always combined with the defeat of regional
lymph glands of the mesentery, and often - and
retroperitoneal glands. On microscopy, they show
the same macrophage reaction as in the lymphatic
intestinal wall apparatus. In enlarged lymphatic
nodes of the mesentery observed foci of necrosis, in some
cases exciting not only the main mass
lymph node, but also passing to the anterior leaf
abdominal covering, which may cause a picture
mesenteric-perforative peritonitis. Can
other lymph nodes - bronchial,
paratracheal, mediastinal. Spleen at
typhoid fever is increased as a result of blood filling and
inflammatory proliferation of reticular cells with
the formation of specific granules. swollen liver,
soft, dull, yellowish on the cut, which is associated with
the severity of parenchymal degeneration. in the kidneys
find cloudy swelling, sometimes necrotizing nephrosis,
less often hemorrhagic or embolic nephritis; not uncommon
inflammatory processes in the urinary tract. IN
areas of hemorrhage appear in the bone marrow,
typhoid granulomas, sometimes - and necrotic foci.
There are degenerative changes in the heart muscle.
Pathological anatomical changes in the lungs with typhoid
paratyphoid diseases are in most cases
inflammatory character. Hyperemia is found
meninges and swelling of the substance of the brain.
salmonellosis
Salmonellosis is an intestinal infection caused by
salmonella; refers to anthropozoonoses.
pathological anatomy
With the most common
gastrointestinal form of salmonellosis
macroscopically revealed the presence of edema, hyperemia,
small hemorrhages and ulcerations in the mucous membrane
gastrointestinal tract. Histologically
found: excessive secretion of mucus and
desquamation of the epithelium, superficial necrosis of the mucosa
membranes, vascular disorders, nonspecific
cell infiltration, etc. In addition to those indicated
changes, in severe and septic forms of the disease
signs of dystrophy and foci of necrosis are often observed
in the liver, kidneys and other organs. reverse development
morphological changes in most patients
occurs by the 3rd week of illness.





![]()

![]()
 Back forward
Back forward
Attention! The slide preview is for informational purposes only and may not represent the full extent of the presentation. If you are interested in this work, please download the full version.
Target:
- to introduce students to information about the main bacterial human diseases,
- continue the formation of the concept and rules healthy lifestyle life
Tasks:
- Find out how pathogenic bacteria enter the human body
- What especially dangerous diseases cause bacteria
- What are the main measures to combat pathogenic bacteria
- How to protect your body from pathogenic bacteria
- Equipment: media projector, ppt presentation
Plan
1. Bacterial diseases human
2. Botulism - causative agent, ways of infection, control measures
3. Dysentery - causative agent, ways of infection, control measures
4. Tetanus - the causative agent, the possibility of infection, preventive measures fight
5. Anthrax - the causative agent of the disease, ways of infection and preventive measures
6. Tuberculosis - the causative agent of the disease, ways of infection, preventive measures
8. Cholera - the causative agent of the disease, ways of infection, control measures
9. Plague - the causative agent of the disease, possible ways of infection, control measures
1. Human bacterial diseases (slide 2)
The number of bacterial diseases in humans is enormous. To date, diseases caused by bacteria are the most dangerous, as they can not only aggravate the quality of human life, but also lead to death. Therefore, we need to know not only the pathogens and symptoms of human bacterial diseases, but also possible reasons these diseases and possible measures fight them. Bacterial diseases include: plague, cholera, anthrax, tuberculosis, botulism, tetanus, tonsillitis, meningitis, diphtheria, dysentery, whooping cough, scarlet fever, gastritis, stomach ulcers and the list goes on and on.
2. Botulism - causative agent, ways of infection, control measures (slides 3-4)
The causative agent is Clostridium botulism, it is widely distributed in nature with a permanent habitat in the soil. It can also be found in manure, fruits, vegetables, fish, excrement of warm-blooded animals. Capable of producing spores that are very resistant to chemicals and physical factors. Spores are able to withstand boiling for 5 hours at a temperature of 120 degrees Celsius. In an environment with a low oxygen content, they multiply rapidly and form a dangerous toxin (poison). Botulinum toxin is one of the known and strong poisons. The pathogen itself does not cause disease in humans, only its toxin is dangerous. For the occurrence of poisoning, it is necessary to multiply the pathogen with the accumulation of botulinum toxin in the body.
It develops as a result of ingestion of food products: ham, sausage, salted fish, as well as canned vegetables, fruits, and especially mushrooms. IN last years cases of botulism in Russia are associated with the preparation of home canned foods. The safety of "jars" can sometimes not be established by eye, botulinum toxin does not lead to a change in the color, smell and taste of food. Swollen cans must be destroyed.
Botulism is a severe toxic-infectious disease that affects the central nervous system, mainly the medulla oblongata and spinal cord. Botulinum toxin is absorbed into the blood in the intestines and selectively affects different departments. nervous system. There is paralysis of the respiratory muscles, muscles of the larynx, pharynx. Cases of fatal poisoning have been reported.
Poisoning develops very quickly, nausea, vomiting, cramping pains in the abdomen appear, liquid stool. At the first sign of poisoning, immediately consult a doctor.
In order not to become infected with botulism, it is necessary: strictly observe the rules of personal hygiene, use only vegetables and fruits, mushrooms that are thoroughly cleaned of dirt for canning. Jars and lids for canning should be washed, scalded with boiling water, and dried. Vegetables, and especially mushrooms, rolled up in jars, cooked at home, are strictly forbidden to buy from random strangers.
3. Dysentery - causative agent, ways of infection, control measures (slides 5-6)
Dysentery is an infectious disease caused by the bacillus dysentery.
Infection occurs when the pathogen enters the body through the mouth with food, water or through dirty hands. Flies can be carriers of dysenteric bacillus. Only people suffer from dysentery. The source of infection may be a sick person. The infection can spread very quickly.
Dysentery is a disease characterized by frequent stools, mucus and blood in the feces, cramping abdominal pain, fever up to 39 degrees or more. The frequency of the chair can reach up to 15-25 times a day or more. The disease is especially severe in children. A child's body dehydrates faster than an adult's. Before, when there were no antibiotics, people died from dysentery.
Treatment of dysentery is aimed at the destruction of the pathogen and it is carried out in an infectious diseases hospital.
Prevention measures: regular and thorough hand washing after using the toilet, walking and before eating, raw vegetables and fruits, get rid of flies in the room, prevent their contact with food. After all, it is not for nothing that dysentery is called the "disease of dirty hands." Currently, you can do a preventive vaccination against dysentery.
4. Tetanus - the causative agent, the possibility of infection, preventive measures (slides 7-8)
Tetanus bacillus is a microscopic bacterium that lives in the gastrointestinal tract of herbivores. Tetanus is acute infectious disease a person, as a result of which the nervous system is affected, the innervation of skeletal muscles is disturbed. Together with the fecal masses of sick animals, a huge amount of spores of the pathogen is released. Spores are very resistant to the effects of environmental factors, they can retain the ability to live for years, being in a state of spores with the soil.
The disease begins acutely. The disease is accompanied by convulsions of skeletal muscles: muscles of the body, limbs, facial muscles, muscles of the pharynx. As a result of the strongest tone and disease state back muscles, then the patient's back arches. The spasm of the muscles is so severe that fractures of the bones and their separation from the bones are possible.
The tetanus bacillus enters the human body through wounds, scratches and other damage to the skin. In some regions, tetanus is referred to as "Bare Foot Disease" because even a splinter in the foot or a rusty nail can become a gateway for infection.
Prevention measures: Reducing injuries, especially when working with the ground (work in mittens or gloves), do preventive vaccinations every 10 years
5. Siberian ulcer is the causative agent diseases, ways of infection, preventive measures (slides 9-10)
Anthrax has been known since ancient times. It is called a malignant carbuncle. The causative agent is a bacterium in the form of a rod, it has the ability to sporulate. Able to survive for decades in the soil or in the tanned skin of sick animals. IN favorable conditions from the spore the bacterium passes into active state. The causative agent of anthrax was first identified by Robert Koch. Until now, anthrax is found in the countries of Central Asia, Africa and South America. It got its name because of its distribution in the past in some regions of Siberia. Now in Russia it is very rare.
The source of infection are sick herbivores: sheep, horses, camels, deer, pigs. Earthworks, soil water during rainstorms and floods contribute to the penetration of bacterial spores into the upper layers of the soil, creating conditions for infecting people and animals. When the disease affects the skin more often. Diagnosis of the disease is not difficult.
Pathogenic bacteria are released into the external environment with the urine of animals, saliva, feces, milk and secretions from wounds. After their death, their organs remain infectious, even the skin, wool and bones. The most common method of infection is contact with sick animals.
At anthrax open areas are more commonly affected body - hands and face. A red spot first appears at the site of the pathogen introduction, in its place a red-cyanotic papule appears over time, which begins to burn and itch, then a bubble appears with liquid, when combed it bursts. The resulting ulcer is quickly covered with a black scab. The lymph nodes are enlarged. The process is accompanied by symptoms of intoxication.
Prevention of the disease is carried out in close contact with the veterinary service.
6. Tuberculosis - the causative agent of the disease, ways of infection, preventive measures (slides 11-12)
The causative agent of the disease is the bacterium tuberculosis bacillus (Koch's bacillus). Tuberculosis sticks are resistant to environmental factors. They can survive in water for up to six months. They remain stable in the dark and in damp for a long time. and at high temperature and sunlight, they quickly die. Until the 20th century, tuberculosis was incurable. The main source of infection, the bacillus excretor, is a sick person. The greatest danger is presented by patients with an open form of tuberculosis. The disease often develops in people who abuse alcohol, and tuberculosis is also widespread in people who are in places of deprivation of liberty (prisons, colonies), or who have recently been released. It is transmitted by airborne droplets, intrauterine infection is also possible.
The main organ of the lesion is the lungs. There are signs by which tuberculosis can be suspected - cough, chest pain, and hemoptysis. Tuberculosis is diagnosed during the passage of fluorography.
The basis of treatment is the use of anti-tuberculosis drugs. The duration of treatment depends on the severity of the disease. In some cases, resort to surgical intervention. Previously, when antibiotics were not known, people died from tuberculosis and called this disease "consumption." Now there is a whole field of medicine dealing with tuberculosis - phthisiology, and its specialists are phthisiologists.
Prevention of tuberculosis consists in the timely passage of fluorography, to give up bad habits - smoking, especially alcohol, to eat right, to lead a healthy lifestyle.
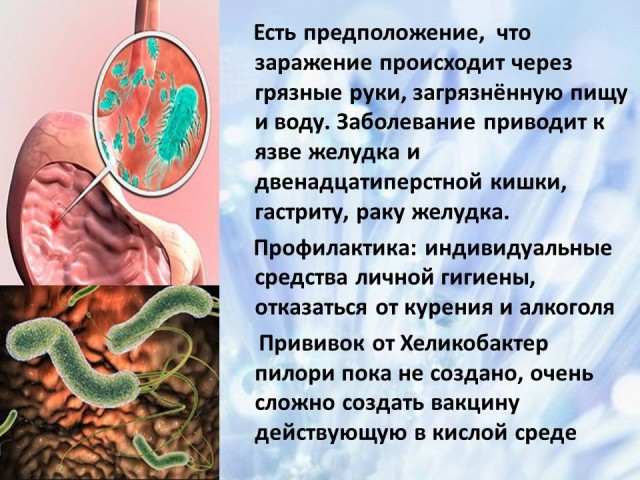
7. Helicobacter pylori - the causative agent of the disease, the possibility of infection, prevention
(slides 13-14)
Helicobacter pylori is by far the most common bacterium. More than half of the world's population can be considered carriers of this bacterium. This bacterium is now the most studied in the world. It is necessary to know what the main signs of infection with the Helicobacter bacterium look like so that treatment can begin in a timely manner. The bacterium lives in the gastrointestinal tract. She feels good in the stomach and is well adapted to aggressive acidic environment stomach.
The exact mechanism of infection is still unknown. There is only an assumption that infection can occur - through dirty hands and contaminated food or water. The disease can be considered familial. As soon as one of the family members becomes infected with a bacterium, then the symptoms of the disease will appear in all other family members
Signs of the disease: problems with the stool (either constipation or diarrhea, heartburn, causeless nausea or vomiting, bad smell from mouth). The disease leads to gastric and duodenal ulcers, gastritis, predisposition to stomach cancer.
Diagnostic methods: gastroscopy with taking a biopsy of the gastric mucosa, fecal analysis, blood test for antibodies. There are many diagnostic methods, but none of them can be considered absolutely reliable.
Prevention measures: personal hygiene products should be individual, wash hands before eating, do not smoke, do not abuse alcohol. Vaccination against the bacterium Helicobacter pylori has not yet been created. It is very difficult to create a vaccine that works in the acidic environment of the stomach.
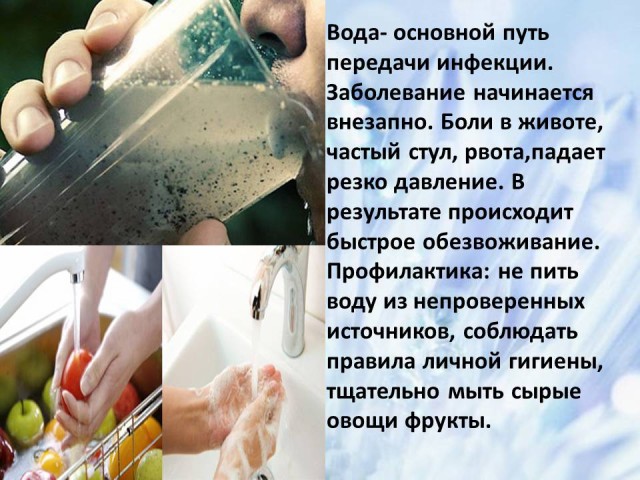
8. Cholera - the causative agent of the disease, ways of infection, control measures (slides 15-16)
The causative agent of cholera is the bacterium Vibrio cholerae. Found in open water sewage, can develop in meat products and milk. According to the World Health Organization, 3-5 million people in the world fall ill with cholera every year. Highly contagious, cholera kills up to 1.5 million children each year. It has been proven that cholera epidemics occur in countries with a low standard of living. More than 2.5 billion people on Earth do not know what a toilet is, they do not even have the opportunity to wash their hands. Flies are carriers of infection. Cholera is a terrible disease that at one time claimed the lives of millions of people. Vibrio cholerae affects the organs of the gastrointestinal tract, mainly the walls of the small intestine.
Water is the main route of infection transmission. Infection occurs through contaminated food, household items, dirty water. The disease begins suddenly. Pain in the abdomen, frequent acts of defecation, thirst, dry mouth, loss of strength, decrease in body temperature, the patient freezes, vomiting appears, blood pressure drops. The result is severe dehydration. The disease is treated with antibiotics.
Prevention measures: do not drink water from unverified sources, follow the rules of personal hygiene, thoroughly wash raw vegetables and fruits.
9. Plague - the causative agent of the disease, possible ways of infection, control measures(slides 17-18)
10. Conclusion(slide 19)
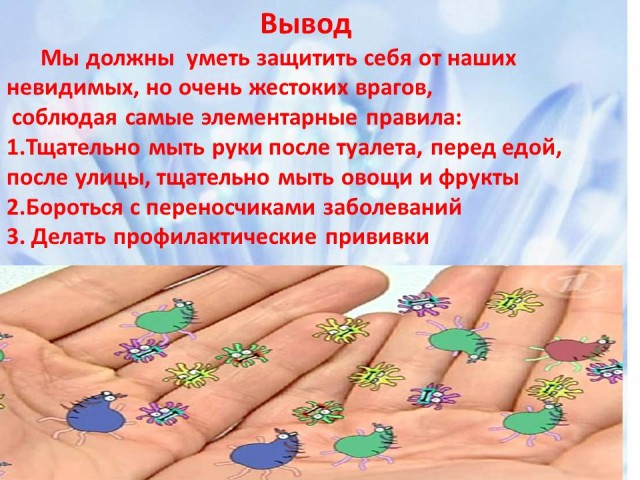
Yes, a person is in danger everywhere, he has a lot of invisible enemies that seek to enter the human body. Therefore, we must learn to protect ourselves from them using the most elementary rules of personal hygiene - wash our hands thoroughly after using the toilet, before eating, after the street, wash vegetables and fruits before eating, follow all the rules of heat treatment when preserving food, fight insect vectors of bacterial infections and rodents, to do preventive vaccinations.
Compliance with these elementary life rules will help you maintain health from a young age and for many years to come. After all, it is neither bought nor sold. Take good care of your health!
INFORMATION SOURCES:
1.http://diagnos.ru
2. http://mymedicalportal.net
3. http://womanadvice.ru.ru
4. www. mikrobak.ru
5.www.provizor.com
6. www.factorpop.ru
7. http://medicina.ua
8. http:/www.skalpil.ru
9. www.jobsmediciner.ru
10. Photos and pictures - www.yandex.ru
A small single-celled microorganism is equally adapted to living in aquatic environment, soil and air space. Look at bacteria normal conditions it is forbidden. Exclusively under a microscope. Although they are in environment a huge number, which is in the millions.
Man and bacteria coexist peacefully. Even an absolutely healthy person has plenty of them in the body. The microflora that is present inside human body becomes an excellent habitat for many types of microorganisms. And they are harmless as long as human immunity is strengthened. But under the influence of damaging microbes, the body's defense functions are weakened. That's when bacteria can cause disease, cause irreparable, sometimes, harm to health.
All known species microorganisms were grouped according to hallmarks. Since their diversity is too numerous, all bacteria have an individual shape:
- spherical cocci;
- bacillus or bacillus;
- spirally twisted spirochetes.
- Not all microorganisms are sensitive to the effects of oxygen compounds. This is also their distinguishing feature:
- aerobic. Need oxygen;
- anaerobic. Capable of obtaining sufficient energy without the participation of oxygen microorganisms.
In addition to external and internal composition They are also distinguished by the way they affect the human body:
- pathogenic. They participate in the process bacterial infection. Or by contact, or from the external environment;
- conditionally pathogenic. They are constantly in the body. They cause diseases only under the influence of certain conditions, such as a decrease in immunity, the penetration of microbes;
- non-pathogenic. adjusted to normal healthy microflora organism. They are not sources of disease, exclude interaction with other microbes and viruses.
These are the microorganisms that actually exist: useful and dangerous. They are not all the same, so do not confuse them.
The process of bacterial infection
The decline in immunity caused by infections will certainly lead to activation. But not all of them are only in our body. Many of them enter the human body from the outside:
- traditional for viruses and infections - airborne method of infection of the body. Occurs through the ambient air by aerobic representatives, as well as through dust in poorly ventilated areas; through objects of common use. Hygiene products, towels, toys, dishes;
- water environment. Naturally, water bodies are polluted with waste and the consequences of improper human activity. This also applies to poorly boiled drinking water, wells;
- soil interaction. These are suburban areas, suburban areas, flower beds. Putrefactive bacteria live here;
- products. wild yeast, mold, salmonella;
- defeat of the fetus of the unborn child in the womb;
- sexually.
In order for the process of bacteria to enter, certain conditions are necessary. Provoke infection:
- decline in immunity;
- warm or hot season. Bacteria are temperature sensitive. An indicator of +4 ° C is considered ideal; a large number of individuals.
To avoid the consequences of the penetration of pathogenic bacteria, vaccination can be carried out, which will prevent their development in the body and produce antibodies.
Intestinal bacteria in the human body
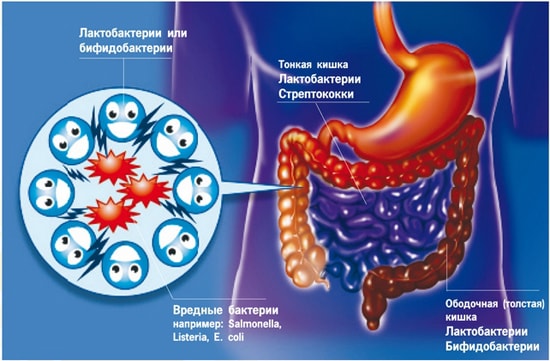
Microorganisms live in the normal healthy microflora of the gastrointestinal tract. They peacefully coexist with the human body. What is healthy intestines and its natural microflora:
- bacteroids. Can provoke the appearance of toxic infections, abscesses, pneumonia;
- bifidobacteria. They prevent the entry of toxins from the external environment. Protect and prevent the growth and spread of pathogenic and opportunistic microorganisms, enhance the synthesis of protein, nicotinic, folic, pantothenic acid, riboflavin, thiamine or B vitamins. Activate the ability of the intestinal mucosa to absorb vitamin D, iron and calcium;
- enterococci. Causative agents of heart problems spread through the blood;
- clostridia. The source of the strongest poison is botulinum toxin. Poisoning results in severe illness like tetanus and gas gangrene;
- pathogens, enterobacteria. The prominent representatives of this group are the plague, coli, salmonella and others. Disrupt the work of all body systems, destroy tissues;
streptococci. Contribute to the appearance pneumococcal infections, toxic damage to internal organs; - staphylococci. Can cause purulent inflammatory infections, sepsis, conjunctivitis. Leads to diseases of the genitourinary system;
- lactobacilli. They are lactic acid bacteria. Normalize stable intestinal microflora.
All of the above microorganisms constantly live in the human gastrointestinal tract. In a healthy person, they do not appear, since bifidobacteria and lactobacilli inhibit them and activate protection.
What bacteria cause bowel disease

Not all microorganisms are equally useful and harmless. Some of them are in external environment, but when ingested, they lead to infectious inflammatory processes. They can also enter other organs. Then they become dangerous:
- Escherichiosis. Become the cause of diarrhea, inflammation of the mucous membrane of the colon. Provoke colitis, acute intestinal infections. Can be transferred to other organs and cause sepsis, pneumonia;
- Coli infection. The main sources of manifestations of enteritis, gastroenteritis, dysentery. Complications occur in the form of cystitis, meningitis, vomiting, strong pain in the abdomen.
Pronounced indicators of the presence of bacteria in the human body are possible diseases they call:
- Peretonitis. The entry of pathogenic bacteria and intestinal microflora into abdominal cavity from the gastrointestinal tract;
- Colpitis. The source of the appearance can be bacteria, such as streptococci, staphylococci, Haemophilus influenzae, chlamydia, Trichomonas. It proceeds as an inflammation of the vaginal mucosa. Penetrates into female organs reproductive system through infection through sexual intercourse. The consequences can be infertility, erosion of the cervix;
- Prostatitis. Infectious way infection involves the penetration of intestinal and Pseudomonas aeruginosa, as well as bacteria, such as enterococci, Klebsiella, into the pelvic organs;
- Dysbacteriosis. It is observed when the microflora is inhibited by potent antibiotics.
To get rid of them, you need a medical qualified help. All microbes, viruses and infections are eliminated only with the help of antibiotics and complex restorative therapy, which is prescribed by the appropriate specialist.
What bacteria live in the mouth
Microflora oral cavity, of course, can not do without its inhabitants. They can be expressed by diseases and emit an unpleasant odor, as well as just being and doing nothing. Do not forget that only in the absence of proper immunity, diseases caused by certain bacteria progress:
- half of the microflora is made up of streptococci. They populate almost the entire body: respiratory organs, gastrointestinal tract, reproductive system and skin cover. But in a healthy person, they do not appear. With a decrease in the body's defenses, bacteria lead to tonsillitis, pneumonia, peritonitis, boils, scarlet fever, rheumatism and toxic shock. This list is quite large. Until defeat of cardio-vascular system and kidneys. They cause the main harm to tooth enamel, lead to caries;
- Pneumococcus. Children's institutions become the most favorable environment for its launch. It is the child who manifests pneumonia, peritonitis, middle ear disease. In heavy running forms many diseases that cause certain bacteria begin to actively progress. The result is meningitis, arthritis;
- gingivalis. They do not act until a certain point, although they are constantly in the mouth. They provoke only inflammation of the tissues around the tooth, periodontitis;
- treponema denticolus. The gums became their habitat. Become the cause of periodontal disease under certain conditions.
These bacteria, unfortunately, cause most of the diseases that occur in the oral cavity associated with teeth and gums.
Bacteria can live on the skin

The skin has become the most favorable place for microorganisms. This and hair follicles, and keratinized areas, and numerous folds. The bacterial layer located on the surface of the epidermis is quite dense.
- streptococci. Bacteria common in almost all systems. But there are many of them top layer epidermis. Lead to toxic poisoning skin. Able to provoke purulent formations. Associated symptoms headaches, vomiting, nausea and sharp rise temperature. Worse the condition in diseases like tonsillitis;
- skin staphylococci, disease-causing like cellulitis, mastitis, abscesses, styes. When exacerbations spread sepsis, toxic shock. Also often provoke a bacterial type of arthritis, diseases of the urinary system, joints, muscle tissue;
You cannot completely get rid of them. They live on a person all his life from the moment of birth and do no harm until favorable conditions for this occur.
Diseases can be caused by fungi on the skin
Mold is also related to bacteria. Molds are often referred to by their characteristics as bacteria. Skin diseases equally can be called by these two representatives. Fungi are located mainly in the same places where other microorganisms of the epidermis live: on the folds, at the base of the hair, in the area of dead skin:
- trichophyton. They affect unprotected parts of the body, live in hay, straw. Lead to dermatological diseases in the area of the knees, buttocks, spread gradually throughout the body;
- yeast provoke lichen, seborrhea. Observed in areas of the head, beard, eyebrows, in the anus;
- known representative of the genus Candida. It becomes the cause of candidiasis, which harms not only the skin, but also the mucous membranes of external and internal organs. Often leads to mycoses. In children provokes diabetes, goes into somatic pathology;
- genus Trichophyton rubrum. Causes diseases affecting the surfaces of the feet, areas between the fingers, nails, gradually covers the entire body;
- Pityrosporum orbiculare. These fungi spread to areas where sebum accumulates. Violate full time job sebaceous gland;
- dermatophytes. Fungal and dermatological problems are typical for widespread these representatives on the skin;
- microsporum. The carrier of this genus of fungi are stray dogs and cats. Children are more susceptible to infection by these representatives. The lesion occurs in the area of vellus hair.
Bacteria that cause diseases

Infectious diseases caused by microbes are quite common. When interacting and favorable conditions amaze important systems in the human body. They can be conditionally divided according to distribution in the body:
- respiratory diseases;
- intestinal infections;
- diseases of the circulatory system;
- skin infections;
- sexual inflammatory processes and others.
Consider the most dangerous and those that doctors most often have to deal with. These main infectious diseases caused by bacteria.
Whooping cough. The cause is the Borde-Jangu bacterium. Appears in strong persistent cough. Seen in younger and older children school age. Transmitted through the air. Duration - up to 14 days.
Tuberculosis. The disease is caused by Koch's wand. Affects the lungs, less often - digestive tract. The patient has cough, sweating, fever. Runs in an open closed forms. Infection is possible by airborne droplets.
Gonorrhea. Infectious lesions of the genital and urinary organs, less often - the rectum and oropharynx. The disease is caused by gonococcus. Refers to venereal diseases. Transmission occurs in the process of intimate contact.
Syphilis. The bacterium Treponema pallidum is the carrier of this venereal infection. It leads to a violation of the mucous membranes of the genital, urinary organs, bones, nervous system.
Tetanus. It can be caused by microorganisms and acquires sharp shape infection skeleton, muscles, nervous system. Immunity to tetanus does not develop. After recovery, I recommend getting vaccinated to prevent re-infection.
Cholera. The causative agent is Escherichia coli Vebrio cholerae. The fecal-oral route of entry into the body is characteristic. Provokes watery diarrhea, dehydration, death.
Common food poisoning caused by bacteria. main reason- salmonella. Fall into digestive system and leads to intoxication of the body and the gastrointestinal tract.
Dysentery. call can intestinal infection Shigella, Shigella. Poisons the body, affects the intestines and stomach, leads to a decrease blood pressure, the appearance of mucus in feces, spotting and an increase in temperature.
